Endotracheal Tube Size Calculator
With our endotracheal tube size calculator, you can now choose an optimal intubation tube for your patients. It doesn’t matter whether they are adults or children. We have got you covered for all of them!
In the text below, you will learn what an ET tube is and how to perform correct endotracheal intubation. After reading, you will also know what methods are used to check if the end of the endotracheal tube is in the right place. Finally, you will get familiar with the ET tube size formula used in our endotracheal tube size calculator.
For more intensive pediatric care, check out our pediatric blood transfusion volume.
💡 The abbreviation ET is formed from the word "EndoTracheal".
We try our best to make our Omni Calculators as precise and reliable as possible. However, this tool can never replace a professional doctor's assessment. If any health condition bothers you, consult a physician.
What is endotracheal intubation?
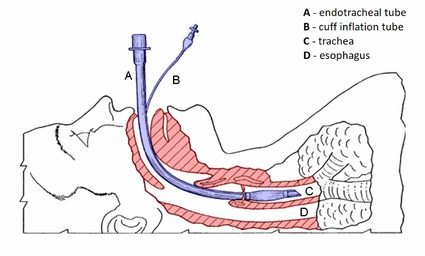
Endotracheal intubation is a medical procedure in which a doctor, normally an anesthesiologist, inserts a special plastic tube – an endotracheal tube – into a patient's airways. Thanks to that, they achieve two major goals.
Firstly, they ensure that all of the air pumped during ventilation (e.g., with an Ambu bag) goes directly into the lungs of the patient. In comparison, when ventilating through a mask that we put on the patient’s face, there is a huge air leak. The air escapes through gaps between the mask and the patient’s face or goes through the throat into the patient’s stomach.
Secondly, they completely seal the airways. The only way for the air to get inside is through the insides of the ET tube. This is prevention against asphyxiation – a situation in which contents of the stomach go back through the esophagus (basically vomiting) and get sucked into the respiratory tracks of the patient.
The patient can also asphyxiate with blood (e.g., from a nose bleeding) and other substances that get into his mouth, nose, and throat. Endotracheal intubation is also performed before surgical procedures requiring general anesthesia. Thanks to that, an anesthesiologist can precisely control the quality of ventilation throughout the operation and administer drugs in gas form in the correct dosage (check out our article and calculator on pediatric dose of paracetamol).
How to perform the endotracheal intubation
Here are the steps to perform an endotracheal intubation:
-
Get all the necessary equipment: gloves, laryngoscope (a device used to make the entry to the larynx visible for a person performing intubation), an ET tube of the corresponding size (acquired thanks to our calculator!), syringe used to inflate a cuff of the endotracheal tube (if it has one).
-
Make sure that the patient is correctly sedated.
-
Stand behind the patient's head.
-
Open their mouth and move the tongue to the left with the laryngoscope.
-
Insert the laryngoscope further into the patient's mouth and try to make the entry to the patient's larynx visible (between their vocal cords).
-
Try to place the end of the ET tube inside the patient's larynx.
-
If successful, inflate the cuff, sealing the airways and preventing asphyxiation.
-
Check whether the patient has been intubated correctly! It is a common mistake to accidentally place the end of the endotracheal tube inside the esophagus instead of the larynx:
-
Place your stethoscope on the patient's stomach and check if you can hear bubbling-like noises. It means that air is going into the patient's abdomen, and you need to intubate again.
-
Place your stethoscope on both sides of the patient's chest. You should hear a symmetrical sound of air going through the bronchi and filling the lungs.
-
Use a capnograph to check if the patient exhales air containing carbon dioxide. The exhaled air should have a higher level of carbon dioxide because it receives it from blood flowing around the alveoli inside the patient's lungs.
-
If still in doubt, perform a radiological test, e.g., a chest X-ray.
-
It is often needed to intubate pre-term babies in the maternity ward as they have difficulty breathing alone. You should individually assess each case. Check out our APGAR score calculator to learn more about evaluating the infant's condition.
Why is it important to choose the optimal size of the intubation tube?
Insertion of an oversized tube may lead to a sore throat and bleeding gums. Keeping an ET tube that's too big inside a patient's larynx for a more extended period can have more severe consequences: damage to the vocal folds, resulting in a change of one's voice and hoarseness, or a laryngospasm (potentially life-threatening contraction of vocal folds). Laryngospasm is dangerous, especially after removing the ET tube, because it is the only thing preventing total contraction of the larynx and suffocation of the patient.
Undersized intubation tube will be ineffective in ventilating the lungs because air will leak around it and go somewhere else, e.g., the patient's stomach. Endotracheal tubes that are too small also tend to slip out of the airway. It can give us a symptom of a sudden decrease in the patient's saturation (hemoglobin oxygenation level), and we will not be able to hear the sound of air flowing inside the patient's lungs.
Uncuffed and cuffed ET tubes
The endotracheal tube (ETT) may be equipped with an inflatable plastic balloon (cuffed ETT), which, when inflated, stabilizes the device in place. Additionally, it seals the airway and protects them from unwanted material (e.g., stomach contents, blood, saliva) getting inside.
Cuffed ET tubes for most ages, except newborn infants (), and are preferred by the hospital workers. For easier insertion, a stylet can be used to stiffen the tube and mold it to a desirable shape.
ET tube size formula
There are many ways to choose an appropriate endotracheal tube size. The most common estimate comes from , which is appropriate for children 1-12 years old. Our calculator combines Cole's formula with for ease of use.
Cole's formula is presented as follows:
size uncuffed = (age / 4) + 4
size cuffed = (age / 4) + 3
The result is the tube's internal diameter in millimeters (mm ID). The cuffed ET tube has to be smaller in diameter (typically by 0.5-1 mm) than the respective uncuffed tube, to account for the size after cuff pressurization. Unfortunately, when we're older, physical development slows down. Because of that, it is easier to predict endotracheal tube size from height and weight, not age alone. This is why – all too often – the ET tube is chosen by trial and error. However, there are more and more ways of estimating the correct size.
Other methods
Different cases call for different ways to estimate the tube size. An overweight, short boy, will require a differently sized ET tube than a slim, tall girl of the same age. A more complex and flexible ET tube size formula for pediatric patients is – taking into account age, height, and weight:
2.44 + (age × 0.1) + (height × 0.02) + (weight × 0.016)
There are many examples of such equations construed for individual variables. For example, evidence shows that body length correlates much better with ETT size than age. For this reason, the allows us to rapidly estimate the equipment size and drug dosages based on the height. The same approach is represented by .
Another important parameter is insertion depth ("tip to lip", calculated from the distal end of the tube to the front of the patient's lip). A quick rule of thumb is that the insertion depth in cm should be approximately three times the ETT size. However, our calculator uses an :
insertion_Depth = (age in years / 2) + 12
These simple formulas will help every emergency medicine and anesthesiology professional be knowledgeable when it shows and effective when it counts.