Light's Criteria Calculator for Pleural Effusion
This Light's criteria calculator allows you to determine the type of pleural fluid - transudate vs exudate - with just a few basic laboratory parameters. Read on to find out how the criteria were built and what are the most frequent pleural effusion causes - you might be surprised that the kidneys and the liver can have something do to with the lungs! At the end, you will also find a quick note on pleural effusion treatment.
We try our best to make our Omni Calculators as precise and reliable as possible. However, this tool can never replace a professional doctor's assessment. Before administering any drugs, fluids, or treatment to your patient, make sure you know the dose and the method.
How to use Light's criteria calculator?
Light's criteria is used to determine if the pleural effusion is transudate or exudate.
Using our calculator is very simple if you provide it with your most recent laboratory test result. Follow these steps:
- To use this Light's criteria calculator properly, you have to have two laboratory test reports. One should be a blood sample, and the other a pleural fluid examination. Make sure you have the right parameters and that they were tested at the same time.
- Type in the pleural fluid and the serum protein concentration. You can switch freely between available units.
- Type in the lactate dehydrogenase concentrations - both in serum and pleural effusion. It only comes in units per liter.
- Fill in the field with the lactate dehydrogenase upper normal limit. It varies very much between individuals and laboratories; that's why we don't provide a range here.
- The calculator will count the criteria and give you a ready answer. Now your transudate vs. exudate dilemma is solved!
parameter | exudate | transudate |
|---|---|---|
fluid protein/serum protein | ≥0.5 | <0.5 |
fluid LDH/serum LDH | ≥0.6 | <0.6 |
fluid LDH/upper normal limit LDH | ≥0.67 | <0.67 |
Pleural effusion - transudate vs exudate
According to scientific definitions, exudate is a fluid arising from inflammation, which damages blood vessel walls, and transudate is a fluid that passes through healthy blood vessel walls.
Stating if the fluid has transudate or exudate features helps you narrow the list of possible causes and start the right pleural effusion treatment as fast as possible.
After getting the lab report, using the Light's criteria calculator should be your next step. With this tool, you can also use other parameters that are beneficial but not included in the pure criteria itself:
- fluid protein - exceeds 35 g/dL in exudates; in transudates usually doesn't go over 25 mg/dL
- fluid cholesterol - over 45 mg/dL (1.16 mmol/L) in exudate; lower in transudate
- the ratio of
serum bilirubin/fluid bilirubin- is greater than 0.6 in exudates and smaller in transudates - fluid appearance - an exudate would be cloudy
Pleural effusion differentiation
What's interesting is that pleural effusion evaluation doesn't have to start with laboratory analysis - even simply looking at the fluid is beneficial and gives you a few clues. For example - if you see a bloody fluid, you should immediately think about trauma, malignancy, or pulmonary embolism. If the fluid is cloudy, it means it's full of triglycerides, which implies chylothorax. If the odor of the effusion sample is hard to stand, it is very likely an infection - probably an anaerobic one.
After that, you can run laboratory tests based on your suspicion. As well as using this Light's criteria calculator to determine if the fluid is transudate vs exudate, you can also examine glucose, fluid pH, or the appearance of special enzymes.
The table shows a list of measured parameters with red light values and possible pleural effusion causes.
laboratory test | abnormal value | possible causes |
|---|---|---|
pH | <7.2 | parapneumonic effusion complication, pleural empyema, esophageal rupture |
glucose | <3.4 mmol/L ( <60 mg/dL) | parapneumonic or malignancy effusion, pleural empyema, tuberculosis |
<1.6 mmol/L ( <29 mg/dL) | pleural empyema, rheumatoid arthritis | |
triglycerides | >1.24 mmol/L (110 mg/dL) | chylothorax (when no cholesterol crystals are present) |
cholesterol | >5.18 mmol/L (200 mg/dL) and crystals | pseudochylothorax |
amylase | increased activity | acute pancreatitis, esophageal rupture, pleural tumors (especially adenocarcinoma) |
adenosine deaminase – ADA, ADA-2 isoform increases specifity | increased activity | tuberculous pleuritis |
hematocrit | ≥50% of peripheral blood hematocrit | pleural hematoma |
neutrophiles | present | bacterial infection, pulmonary embolism |
lymphocytespresent | tuberculosis, malignancy | |
eosinophiles | >10% | asbestosis, malignancy, parasite infection, Churg-Strauss syndrome, drug-induced reaction, blood or air presence in the pleural cavity |
If you're interested in laboratory analyses, check our absolute lymphocyte count calculator, absolute eosinophil count calculator, and serum-ascites albumin gradient calculator that analyses the ascites fluid.
Pleural effusion causes
Pleural effusion is not a diagnosis in and of itself - it's just a sign. You have to find the underlying cause and treat it to prevent a recurrence properly. The table shows the most frequent causes of both transudative and exudative pleural effusions.
exudative effusion | transudative effusion |
|---|---|
pneumonia | heart failure |
malignancy (pleura, breast, metastases) | |
infections (incl. tuberculosis) | nephrotic syndrome |
peritonitis | heart diseases (pericarditis, mitral valve stenosis) |
rheumatic diseases (lupus, sarcoidosis, immunological vasculitis, rheumatoid pleuritis) | hypoalbuminemia – would cause effusions in other body cavities as well |
pancreatitis | atelectasis |
pulmonary embolism | hypothyroidism |
pulmonary infarction | peritoneal dialysis |
ARDS – acute respiratory distress syndrome | urinothorax |
lung abscess | |
esophageal rupture | |
chylothorax |
Pleural effusion treatment
As mentioned above, pleural effusion treatment is basically finding the underlying disease and treating this condition. However, in some cases, we would like to address the effusion itself during therapy.
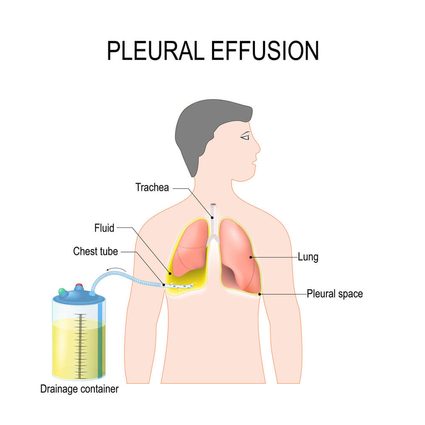
A small amount of fluid would absorb on its own, but in cases where a larger amount is present, especially if it is severely affecting the patient's state, we would drain the fluid. Drainage means putting a little plastic tube (called a drain) into the pleural cavity so that it allows fluid evacuation. Sometimes we would just do it once - a procedure called puncture, sometimes it requires leaving the drain in for some time.
If the effusion source is constant and untreatable (like a palliative state of cancer) and the fluid severely affects the patient's wellbeing, a procedure called pleurodesis should be performed. Pleurodesis means an artificial obliteration of the pleural cavity - sticking the two layers of pleura together. Actually, it means there is no pleural space after pleurodesis, so there is no place for the fluid to collect.
To achieve that, we use either chemical or physical agents. Some examples include talc, bleomycin, and tetracycline. Sometimes surgical methods, like mechanical pleura irritating, are used.
A note for the patient - why is there water in my lung?

If your doctor tells you that there is a fluid in your lung, they don't mean a specific disease called 'pleural effusion' - there is no such diagnosis. Water in your lung is just a symptom of something else. But how does it get there?
The fluid of ~10 ml in the pleural cavity is natural and healthy. Even in this small amount, it prevents unnecessary friction between the pleura and the lungs during regular breathing. The fluid is an infiltrator, coming from microcirculation vessels in the pleura and going to lymphatic vessels. It circulates all the time but stays the same amount.
There are a few causes of accumulation of fluid in the pleural cavity:
- Increase in the hydrostatic pressure in vessels
- Decrease in the oncotic pressure in vessels
- Decrease in the hydrostatic pressure in pleura
- Increased permeability of the pleural vessels
- Lymphatic vessels occlusion
- Fluid movement from the peritoneum
Hydrostatic pressure - is the pressure of the fluid and depends mainly on fluid density. The larger the gradient of hydrostatic pressure on both sides of the vessel wall, the faster the fluid movement will be. In the case of pleural effusion, this mechanism is responsible for fluid accumulation caused by heart failure (increase in hydrostatic pressure).
On the other hand, a decrease on the other side of the pleural vessels will have the same result. It happens, e.g., in atelectasis.
Oncotic pressure - is pressure dependent on serum proteins, which kind of 'attract the water to themselves. Normally, there are more proteins in serum than in the extracellular fluid (ECF), but, in states of decreased protein production like liver failure, or increased protein loss (nephrotic syndrome), the quantity of proteins in ECF outbalances the amount in the serum. This causes the fluid to escape the vessels.
Increased permeability - a simple inflammation is responsible for increased permeability, so that we would include pneumonia here. Another main cause is ARDS - acute respiratory distress syndrome.
Fluid movement from peritoneum - in the case of ascites, positive pressure in the peritoneal cavity can force fluid to move to the pleural cavity.
Lymphatic vessels occlusion - in a healthy state, pleural fluid circulates all the time, and its way out is through the lymphatic system. In the case of lymphatic vessel blockage, e.g., by malignancy cells or pressure on vessels of some kind, the drainage is impaired.